What causes athlete’s foot?
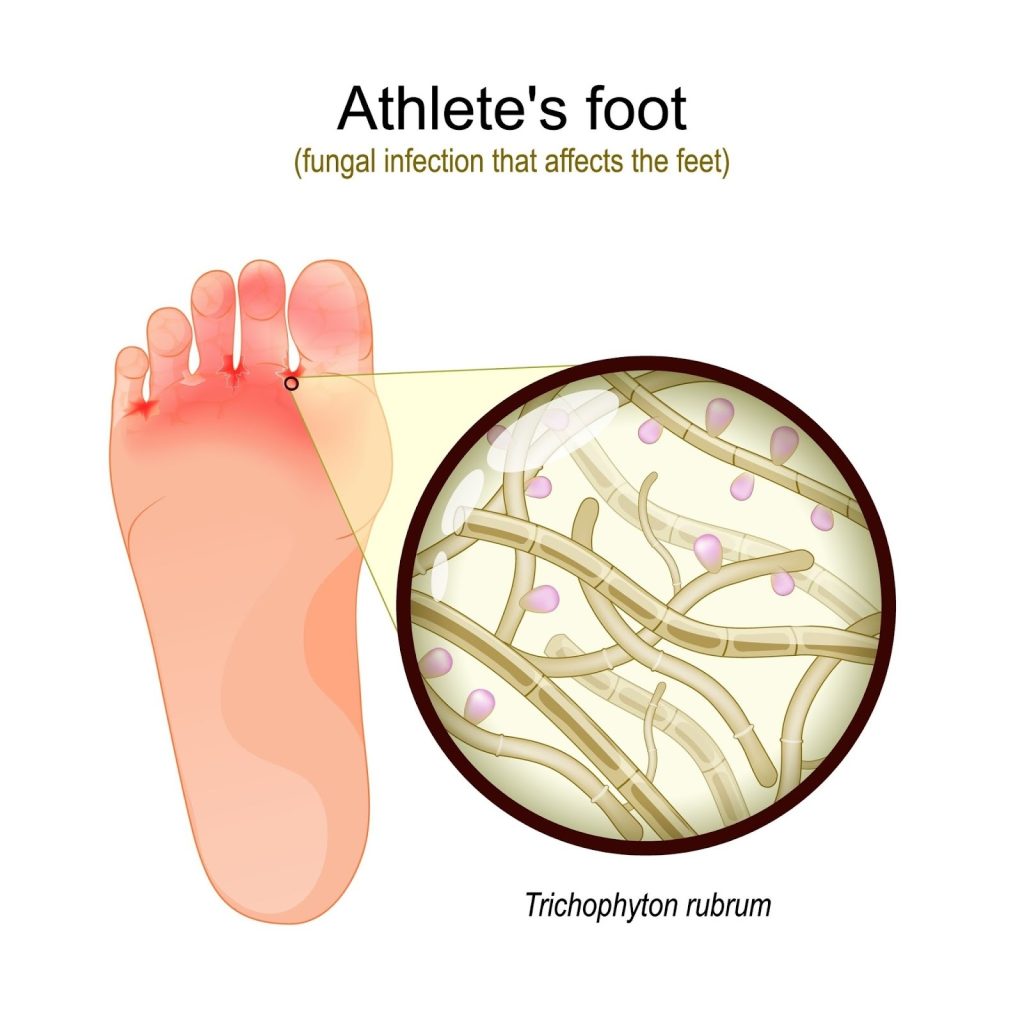
Athlete’s foot is caused primarily by dermatophyte fungi, the same type of fungus responsible for many common skin infections. These fungi thrive in warm, moist environments and can easily multiply when the skin stays damp for long periods. Once they enter the outer layers of the skin, often through tiny cracks or weakened areas, they begin to grow and spread.
Common factors that increase the risk of athlete’s foot include:
- Damp socks or shoes that trap moisture around the feet
- Sweaty feet, especially during exercise or long hours in enclosed footwear
- Walking barefoot in communal areas such as pools, gyms, or shared bathrooms
- Sharing towels, shoes or socks with someone who has a fungal infection
- Dry or cracked skin that allows fungi to enter more easily
- Reduced immunity, which makes it harder for the body to fight off fungal growth
What are the signs and symptoms of athlete’s foot?
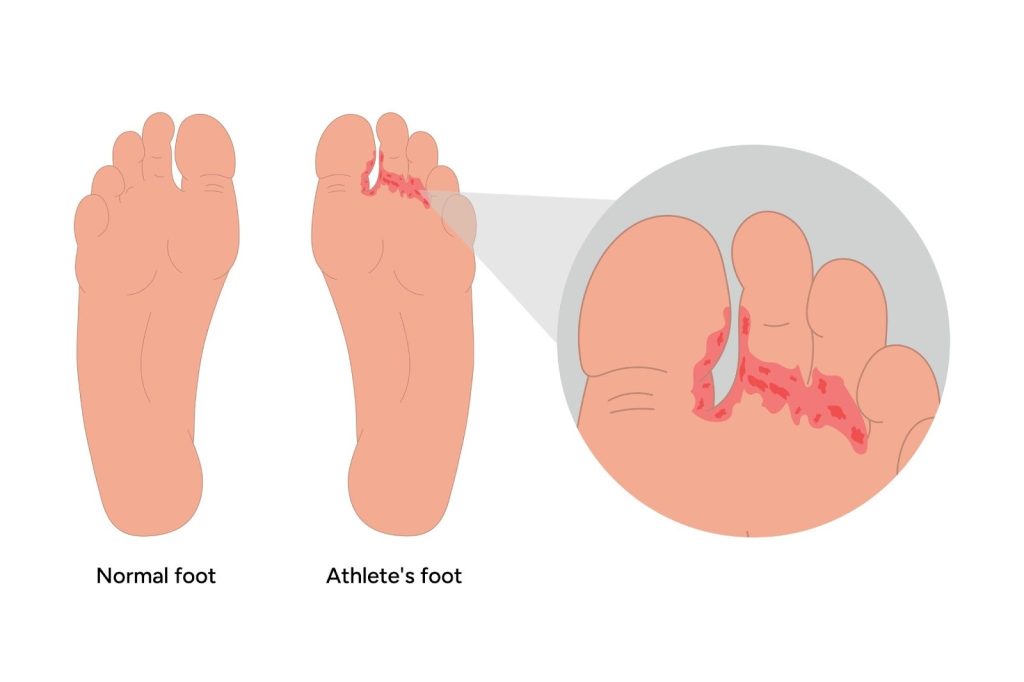
Athlete’s foot can present in several ways depending on how the fungus affects the skin. Some people experience mild irritation, while others develop more noticeable inflammation or cracking. Recognising the early symptoms helps prevent the infection from spreading or becoming chronic.
Common signs and symptoms include:
- Itching or burning skin, especially between the toes
- Redness or inflammation in affected areas
- Peeling or scaly patches that may feel rough or flaky
- Cracked or painful skin, sometimes leading to soreness when walking
- Small blisters or watery bumps that may break easily
- Dry, thick or flaky skin on the soles (often called the moccasin type of athlete’s foot)
What happens if athlete’s foot is left untreated?
Athlete’s foot may start as mild irritation, but the infection can gradually worsen if it is not managed early. The fungus can spread to surrounding skin, deepen into cracks and create ongoing discomfort that affects daily activities.
Possible complications of untreated athlete’s foot include:
- The infection spreading to other toes or both feet, making it harder to treat
- Painful skin cracks, which can lead to deeper bacterial infections
- Fungal spread to the toenails, causing thickening and discolouration
- Increasing discomfort when walking, especially if the skin becomes raw
- Persistent flare-ups or chronic dry, scaly skin that keeps returning
Early podiatry treatment helps control the infection, relieve symptoms and prevent it from spreading to the nails, other areas of the foot or your loved ones.
When should you see a podiatrist for athlete’s foot?
While mild cases of athlete’s foot may respond to basic home care, some infections require professional attention, especially when symptoms persist or begin affecting your daily comfort. A podiatrist can assess the skin, identify any complications and guide you toward the most effective treatment.
You should see a podiatrist if you notice:
- Symptoms not improving with home care after one to two weeks
- Severe itching or burning that affects walking or sleep
- Painful cracks or raw skin, particularly between the toes
- Signs of a secondary infection, such as swelling, pus or increased redness
- Fungal involvement of the toenails, including thickening or discolouration
- You have diabetes or circulation problems, where even minor skin issues need careful management
How is athlete’s foot diagnosed?
Athlete’s foot is usually diagnosed through a simple podiatry examination. The podiatrist will assess the appearance of the skin, the pattern of redness or peeling and whether the infection has spread to other areas such as the toenails. In cases where the symptoms resemble other skin conditions, the podiatrist may advise for a small skin scraping to be taken and sent for laboratory testing to confirm the presence of fungal organisms. This ensures the right treatment is selected from the start.
What are the treatment options for athlete’s foot?
Treatment for athlete’s foot varies depending on how severe the infection is, how much skin is involved, and whether the toenails have also been affected. At Atlas Podiatry, our podiatrist will choose the most suitable approach based on your symptoms and how your skin responds.
- Topical antifungal creams or sprays — these are commonly used for mild to moderate infections. They help reduce fungal growth when applied consistently over several weeks and are often the first line of treatment.
- Oral antifungal medication — for more persistent or widespread infections, oral tablets may be needed. These are arranged in coordination with your general practitioner (GP) and used when topical treatments alone are not enough to control the fungus.
- Professional skin care and debridement — when the skin becomes thick, flaky or scaly, the podiatrist may gently remove the excess skin. This helps antifungal medication penetrate more effectively and improves comfort.
- Management of secondary infections — if cracks, raw skin or irritation are present, the podiatrist will provide guidance to reduce inflammation and prevent bacteria from entering the broken skin.
- Treatment of fungal toenails (if present) — athlete’s foot and fungal toenails often occur together. If the toenails have thickened or become discoloured, separate podiatry treatment may be needed to address the nail infection as well.
Our podiatrist will design a treatment plan that matches your skin type, symptoms, activity level and the likelihood of recurrence, ensuring you receive effective and comfortable care.
How can you prevent athlete’s foot from returning?
Preventing an athlete’s foot from recurring is an important part of long-term foot care. Fungal infections thrive in warm, moist environments, so daily habits play a big role in keeping the skin healthy and fungus-free.
Helpful prevention steps include:
- Keep feet dry and clean, especially between the toes
- Change socks daily, or more often if they become damp
- Choose breathable footwear that allows air circulation
- Avoid walking barefoot in communal areas like pools, gyms, and shared showers
- Use anti-perspirant powders or sprays if you are prone to sweating
- Disinfect shoes regularly to reduce fungal spores
- Keep toenails trimmed and clean, as fungi can infect the nails
- Follow podiatry advice for long-term skin health and to prevent flare-ups
Summary
Athlete’s foot is a common fungal skin infection, and it can quickly become uncomfortable when the skin starts to itch, peel or crack. With the right treatment, most cases respond well and the skin returns to its normal, healthy state. At Atlas Podiatry, care focuses on relieving irritation and preventing the fungus from recurring, or spreading to other areas of the foot or the toenails. Treatment is guided by the severity of the infection and may involve antifungal medication, gentle skin debridement and advice on managing moisture and footwear. With consistent care and simple daily habit changes, most patients experience steady improvement and fewer recurrences.
If you are dealing with persistent itching, peeling skin or suspected fungal infection, schedule a consultation with Atlas Podiatry for professional athlete’s foot assessment and treatment in Singapore.
